During the weekly COVID-19 press briefing on Thursday, August 13, 2020, Governor Gary Herbert interviewed Utah Department of Health deputy director Nate Checketts, who oversees testing for Unified Command. We recognize there are some persistent questions Utahns have about testing for COVID-19. This is a summary of their discussion:
1. Why is testing so critical to our pandemic response?
Testing for COVID-19 is a little different than testing for other diseases. For many diseases, like strep, we test so we can confirm the presence of the disease and begin treatment.
For COVID-19, we test:
- For confirmation of the disease even though there is no treatment that can reverse the infection.
- To help slow its spread to other people.
- To identify positive individuals so our contact tracers can reach out to their close contacts and advise them to follow isolation or quarantine guidelines.
- To help Utahns who were exposed to COVID-19 know what they should be doing to keep their families and communities as safe as possible.
- To help us know how much and where COVID-19 is spreading in order to take appropriate actions.
We cannot stop a disease if we don’t know where it is. With testing, we have data to help Utahns make informed decisions to keep their families safe and help policy makers make decisions about activity levels, masking, etc. If we can stop the spread, we can control the pandemic and keep our economy open. Testing is key to how we do this.
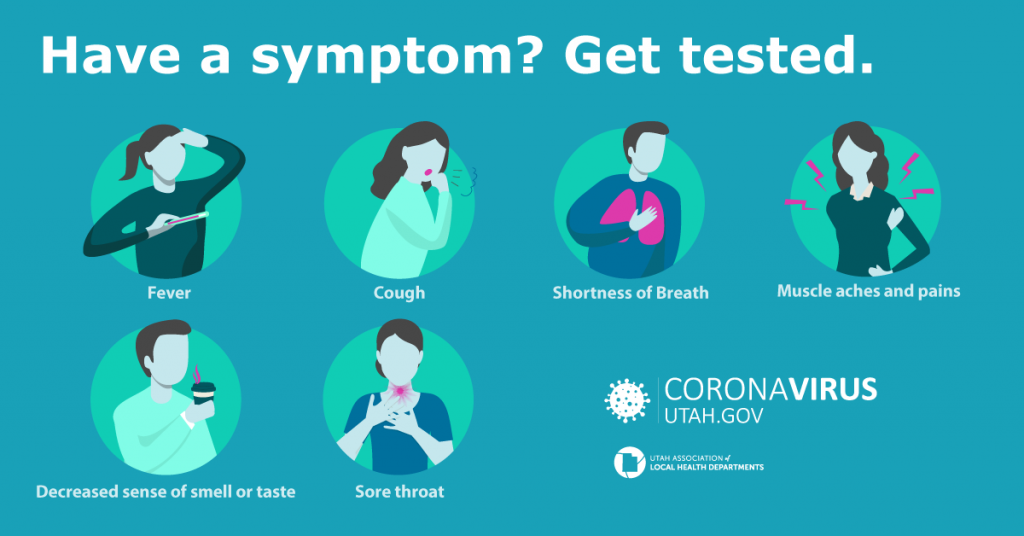
2. Who should be tested?
Anyone with 1 of 6 symptoms consistent with COVID-19 should get tested. These symptoms include a fever, cough, shortness of breath, muscle aches, sore throat, or a loss in your sense of taste or smell. If you have one of these symptoms, even if mild, we encourage you to call a healthcare provider and get tested. You can find a list of testing locations here on the website.
We also recommend you get tested if you have come into close contact with someone who has COVID-19, regardless of symptoms. In these cases, a public health worker will give you a referral code for testing. If a person who was exposed to COVID-19 chooses to get tested, he or she should wait at least 5-7 days after their last exposure to get tested. This lets enough of the virus build up in his or her body to be detected by the test. Getting tested before this time may result in a false negative test result. This means the person tested negative but is really positive and can infect others with COVID-19. However, even if the test is negative, anyone exposed to someone who tested positive for COVID-19 should quarantine for the full 14-day period.
3. Do you have to have a symptom to get tested?
We recommend anyone with COVID-19 symptoms get tested. This is one of the most important things individuals can do to help the state’s response, in addition to quarantining and isolating when asked to do so.
Testing for COVID-19 is most accurate when someone has symptoms. Testing people who are asymptomatic or presymptomatic, meaning they do not have symptoms of COVID-19, can increase the chance of an inaccurate test result.
At this time, asymptomatic testing is primarily available for certain groups of higher risk individuals. Some of these groups include people who had a close contact exposure to someone who tested positive for COVID-19, first responders, long-term care facilities, and areas or facilities where an outbreak has happened or is likely to happen.
It’s always best to call a healthcare provider or testing site first, to make sure you are able to get tested.
4. Let’s talk about the different kinds of tests:
There are two tests that can tell us if someone is infected with COVID-19 and can spread it to others — PCR and antigen. These are key in the state’s response for identifying spread and stopping spread.

PCR test – A reverse transcription polymerase chain reaction (rRT-PCR or just PCR) test looks for the genetic material of the virus that causes COVID-19. Generally, a healthcare worker uses a swab to collect a sample by inserting the swab up your nostril to your throat, behind your nose. PCR tests are very accurate in diagnosing someone with COVID-19. It can take several days to get your test results back with a PCR test, depending on which lab your healthcare provider sends your sample to and current testing demand.
Antigen test – An antigen test is often a rapid test where you can get results in minutes instead of days. An antigen test looks for proteins found on or within the virus that causes COVID-19. Like a PCR test, a healthcare worker uses a swab to collect the sample. While antigen tests are accurate and several have been approved by the Federal Drug Administration, there is a higher chance of having a false negative test result than with a PCR test. This means if you test negative for COVID-19 with an antigen test, you may also need to get a PCR test to make sure you don’t have COVID-19.
Serology or antibody test – Serology, or antibody tests, may be able to tell if you have ever been exposed to the virus that causes COVID-19. A sample of your blood is collected and is used to see if your body has made antibodies to the virus. Your body makes antibodies when it fights an infection. Antibodies in your blood mean, at one time, you were exposed to COVID-19. Antibody tests find these antibodies in your blood and tell you if your immune system has responded to the infection. We don’t yet know how long a person is immune to COVID-19 after they are infected or exposed to the virus that causes this disease. This means a positive antibody test does not guarantee immunity to COVID-19. If you test positive for COVID-19 antibodies, we recommend you get a PCR test to know if you are infectious.
5. How does a person go about getting tested?
There are many ways a person can go about getting tested. If you have 1 of the 6 symptoms of COVID-19 eligible for testing in the state (fever, cough, shortness of breath, muscle aches, sore throat, or loss of your sense of taste or smell), we encourage you to call a healthcare provider and get tested. You can find a list of testing sites at coronavirus-stage.at.utah.gov.
A public health worker may also give you a referral code to get tested if you were exposed to someone with COVID-19. They will ask you to wait 5-7 days after you were exposed to get tested. This lets enough of the virus build up in your body to be detected by the tests.
6. Where can people be tested?
There are 76 public testing sites in Utah, which can be found right here:
You can also call your healthcare provider to find out where you can get tested.
7. Can you just show up at a testing location?
It depends on the site. The testing site information on Coronavirus.utah.gov (español) includes whether pre-registration is required at a particular testing site. Most sites encourage registration before coming to the site in order to speed up the process.
8. How much does a test cost?
Most people will not have to pay for COVID-19 testing. You should not be asked for payment when you go to a testing location.
• If you have health insurance:
Families First Coronavirus Response Act ensures the cost of getting a COVID-19 test is covered at 100% if you have health insurance AND you have a medical reason to be tested. This means you have symptoms of COVID-19, you have had close contact with someone who has COVID-19, or you have a referral from a healthcare professional or the health department to get tested.
• If you are uninsured and are a U.S. citizen and a Utah resident:
You qualify for COVID-19 testing coverage through Medicaid. You need to apply for this program at https://medicaid.utah.gov.
• If you are uninsured and do not qualify for the Medicaid option:
There are locations that will provide testing free of charge. If you need help finding a location that provides free testing, please call the Utah Coronavirus Hotline at 1-800-456-7707 or use the chat feature on the coronavirus-stage.at.utah.gov website.
• If you are being tested for employment, travel, or a non-medical reason:
You may be charged for the test. Testing for general workplace health and safety (such as employee ‘return to work’ programs), public health surveillance, or any other purpose not primarily intended for diagnosis or treatment of COVID-19 or another health condition are not included in the requirements of the Families First Coronavirus Response Act.
We have more information on testing and insurance here at https://coronavirus.utah.gov/.
No one should be afraid to get tested because of cost
9. What should a person do if they test positive?
If you have symptoms of COVID-19 or test positive, you should isolate. This means you stay at home except to get medical care. You will need to take extra precautions to keep others who live with you safe, such as wearing a mask when you are in the same room with other people, cleaning surfaces that are touched often (like doorknobs), and staying in a separate room as much as possible.
If you tested positive for COVID-19, you should isolate until your symptoms have gotten better and you are fever-free for 24 hours and it has been at least 10 days since you first got sick or tested positive.
Everyone who lives in your home or who came into close contact with you up to 2 days BEFORE you first got sick or tested positive, should quarantine for 14 days from the last date of their exposure to you.
10. What should a person do if they test negative? Are they out of the woods?
A negative PCR or antigen test does not mean you won’t ever get sick with COVID-19. It only means you did not have the virus at the time of your test. It’s possible that you were very early in your infection and did not have enough of the virus in your body to be detected by the test.
If you were exposed to COVID-19, you should quarantine for 14 days from the last time you were in close contact with the person who tested positive for COVID-19. Public health may recommend you get tested 5-7 days after the exposure. However, even if the test is negative, you must finish the 14-day quarantine. It may take up to 14 days to know if you will get sick.
Everyone, regardless of what their test result is, should still practice good hand hygiene, wear a mask, physical distance, and stay home when they are sick.
11. How many tests can the state handle in a typical day?
Back in March, we were doing 800 tests a day across the entire state. At several labs, extraction of the genetic material from the sample was done through a manual process. There were so few reagents to perform the extraction that we once had a team member drive across the county to meet someone in a parking lot to pick up donated extraction kits to keep the state lab functioning for a few more days.
Now the state lab alone can process 1,200 tests in a day and other labs have significantly grown their capacity too. Right now, lab capacity for tests statewide is about 9,000 per day.
12. We have the capacity to do 9,000 tests a day. But we’re not seeing those kinds of numbers over the last couple of weeks. What can we attribute that to?
It’s difficult to pin down one specific reason why our testing numbers have declined recently. Best case scenario — it’s because people aren’t sick. Our rolling 7-day average for percent of positive laboratory tests has been declining for the last week and we are hopeful this trend continues. We are also seeing a similar decline in COVID-like illness being reported in our syndromic surveillance.
Many of our sample collection sites are reporting fewer people are seeking out testing as well. However, we are still testing around 4,000 people a day and our cases have dropped much faster than testing has declined.
It’s certainly not a time we can ease up on our efforts. All of us have a responsibility to protect our families and communities by practicing good hand hygiene, wearing a mask, physical distancing, staying home when we are sick AND getting tested when appropriate.
13. The Legislative Auditor recently called on the executive branch to improve turnaround times for test results. What are we working on?
During the surge in June and July, testing turnaround times lengthened significantly for many labs locally and across the country. Some providers were warning that results may not be back for 7-10 days. By this point, the value of the results of the tests are extremely reduced for the individual and for possible interventions to slow the spread. Thankfully, turnaround times have improved in recent weeks as the testing surge has lessened. At the state lab, turnaround times this week have been around one day.
We are working with state leadership to set goals for turnaround times. Our goal is that most testing results be provided within 48 hours and that certain high priority groups (like residents of a nursing facility where there is an outbreak) have their results within 18 hours.
In order to improve our turnaround time for the high priority groups, we are:
- Implementing technology improvements (e.g., moving to barcoding).
- Augmenting staff (e.g., adding extra shifts at sample receiving and in the lab).
- Implementing process changes in sample collection (e.g., organizing mid-day couriers if mobile teams won’t be returning to the lab until the evening).
Since the beginning of the COVID-19 response, we have been meeting with our local labs, sample collection sites, and healthcare officials to share best practices, learn from each other’s mistakes, and identify common goals.
14. What does the future of testing look like?
Testing capacity is increasing all the time. We recently completed a solicitation for sample collection and lab partners and will be able to bring online capacity for thousands of more tests.
Governor Herbert signed a letter of intent with several other states to commit to buy at least 500,000 rapid tests. We have already placed initial orders with some rapid test manufacturers and are working to finalize agreements with others.
Additional options for collecting samples, like saliva, have some approved tests and it’s likely we will see others approved soon. And we hear about developing options like low cost paper strips that could detect antigens.
We also hope that manufacturers are successful in their vaccine development efforts and that we will be able to move on to the next challenge of vaccine distribution.
Meanwhile, it’s important to keep transmission low now so we need to keep social distancing and masking. Everyone should also get their flu shot to make sure we stay healthy during this upcoming flu season and don’t clog the emergency rooms when another wave of COVID-19 may hit.
END

