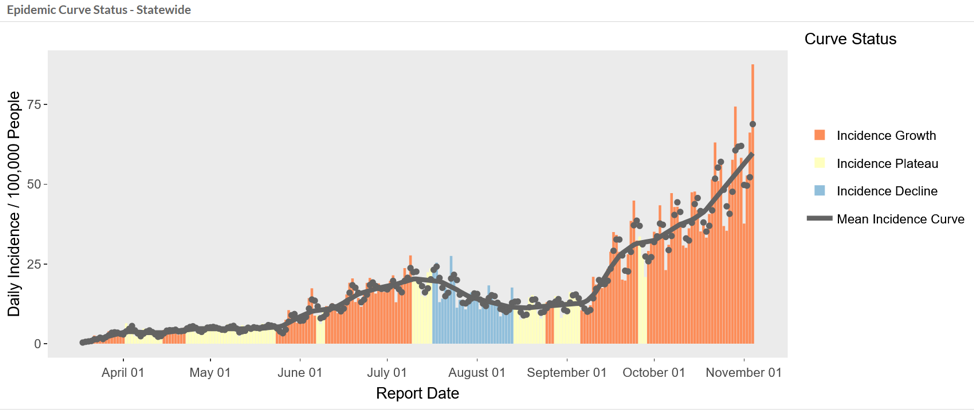
Governor Herbert and Utah’s hospital leaders have been telling Utahns for several weeks that sharply increasing COVID-19 cases could strain Utah’s hospitals beyond their capacity. This chart demonstrates that COVID cases have increased fivefold in only two months between Sept 5th and Nov. 5th.
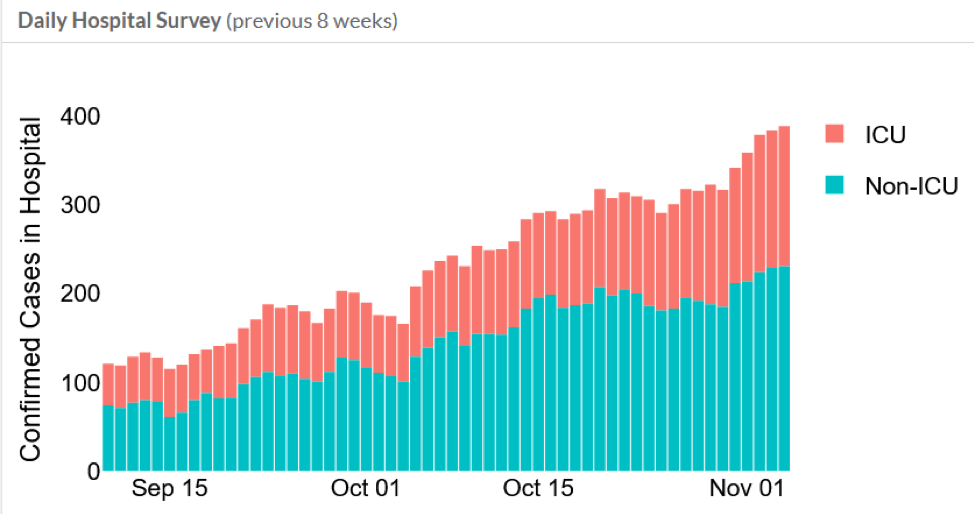
The next figure shows COVID-19 hospitalizations have increased four times (400%) in the same period—the last 8 weeks.
The following chart shows the total number of COVID-19 cases hospitalized throughout the pandemic. About five percent (5%) of Utah’s COVID cases need hospitalization: the more cases, the more demand on hospitals.
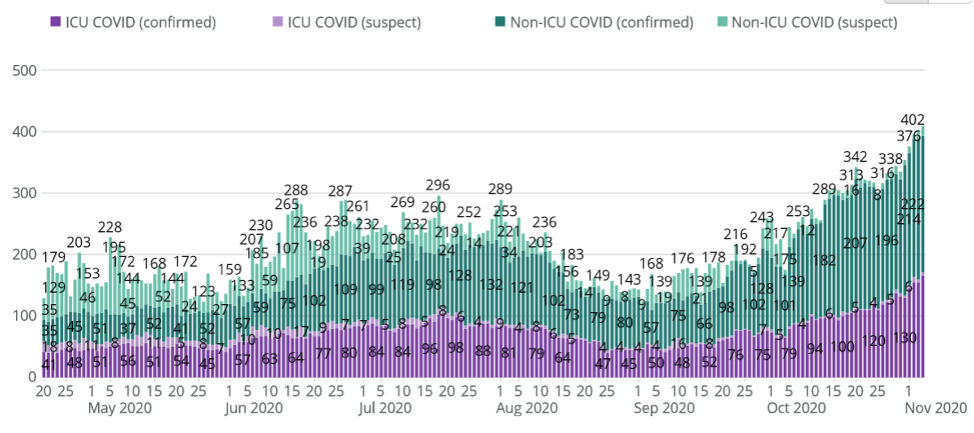
During the July surge, the highest number of COVID-19 hospitalizations was 296. As of Nov. 5th, there were 402 hospitalizations.
The following chart depicts total ICU use for all causes. Throughout the summer, ICU beds were about 70% full. However, beginning in October, 85% of ICU beds have been full. Hospitals ICU units are functionally full when they reach 85%.
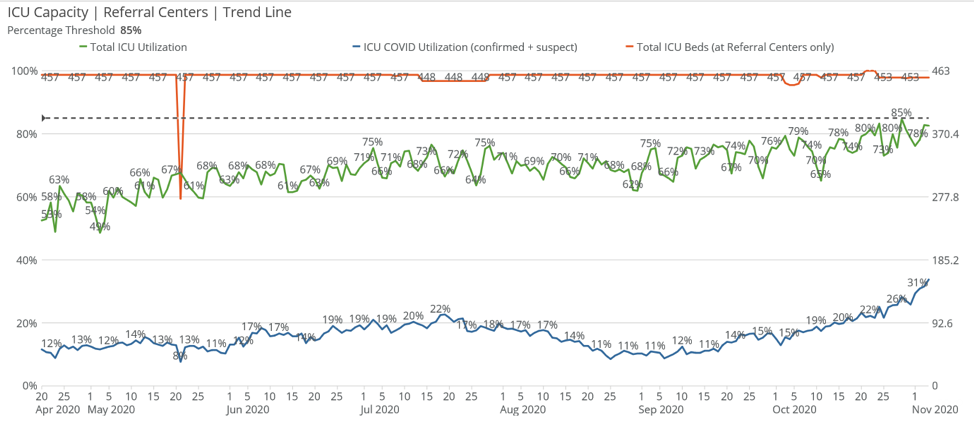
The bottom blue line on the graph above shows the percentage of COVID-19 cases in our ICUs, which increased from the July peak surge of 22% to 32% in early November.
Please remember that before the COVID-19 pandemic, Utah’s hospital ICU units were typically from 60% to 70% occupied by patients with heart attacks, strokes, traumatic injuries and other conditions requiring round-the-clock care from skilled nurses, doctors and technologists. Currently, COVID cases have added another 32% of cases.
Utah’s ICU hospital beds are nearly full.
Utahns frequently ask, “Why are hospitals overwhelmed with COVID patients when I know of hospitals that have only a few COVID patients or none at all, and when you’ve been reporting that statewide ICU utilization is only 70-80%? Doesn’t that mean they have some space left?”
Not all ICU beds are equal.
For many months, community hospitals—including those in rural areas— have been referring COVID patients to higher tier hospitals with expertise, experience and equipment to care for these patients, called “referral hospitals.” While Utah hospitals have about 535 ICU beds, referral hospitals have only 453 ICU beds.
Under normal circumstances regular hospitals take care of most of their own cases, but “refer” complex or more severe cases to the higher tier “referral hospitals.” But in this current major spike in cases, referral hospitals are nearly full. The University of Utah Hospital and Intermountain Medical Center have handled the majority of Utah’s severe COVID cases. Both have been full or nearly full for the last few weeks as have McKay-Dee in Ogden and St. George Hospital in Washington County. The last chart above shows that all referral hospital beds are about 85% full.
Load Leveling Among Hospitals.
The State and the Utah Hospital Association have stood up a virtual transfer command center, which keeps track of ICU and hospital census. Beginning in November, as some hospital ICU units have reached capacity, the command center was called upon to arrange transfers to other hospitals with remaining capacity.
“Beds don’t treat people; people treat people.”
Critical care doctors, nurses and highly-skilled technicians like pulmonary techs have been working nearly round the clock since the pandemic hit Utah last March. They are exhausted and overwhelmed. And as this article explains, we just don’t have enough of them: “Health systems can build more ICU beds and buy more ventilators, but the ICU workforce is less easily expandable. For decades leading up to COVID-19, we have known that a mismatch exists in the U.S. between the need for ICU beds and the number of qualified ICU practitioners. COVID-19 has simply widened this gap.”
At the same time, the constant, intense demand on these professionals, infections and quarantines of front-line healthcare workers, as well as the general life challenges all of us face during this difficult pandemic, have dramatically reduced the available nursing staff as the pandemic drags on. Thus, as we reach maximum hospital ICU capacity, hospitals are making do: 1) doctors and nurses are caring for more patients and work more shifts, increasing the burden on them, and/or 2) the hospital may have to use doctors and nurses that aren’t trained or as experienced in critical care. Hospitals have expanded capacity by building additional temporary ICU beds. Staff have had to work many extra shifts. They’ve brought in other doctors and nurses to supplement regular staff. The state has leased skilled nursing facilities for COVID patient overflow.
In the early spikes in Italy, New York, and elsewhere, there were only a handful of those severe hotspots, so they were able to build field hospitals and bring in doctors and nurses from other areas. Unfortunately, the current surge is a national one, so there aren’t doctors and nurses available to come help. Arizona, Nevada, Idaho, and Colorado can’t send nurses and doctors to help Utah because they’re dealing with their own serious spikes.
In the coming days, rural hospitals may no longer be able to refer serious patients (COVID or otherwise) to referral hospitals but will have to do the best they can to care for them. And even at referral hospitals, patients will increasingly be cared for by doctors and nurses who are acting outside their specialty and/or are caring for more patients than is ideal.
When hospitals get overwhelmed: Crisis Standards of Care.
When hospital resources are maxed out, doctors must make tough choices about who gets scarce attention, drugs and supplies. Years ago, the State of Utah with the Utah Hospital Association drafted Crisis Standards of Care, which guides doctors in deciding who gets care and who doesn’t, based on who is most likely to survive. The Standards have been updated to reflect the unique issues of the pandemic.
Although no one wants to make such choices, our escalating case counts put us on a trajectory that might require it.
Universal Masking Can Avert Disaster.
This dire result can be avoided or lessened dramatically if Utahns wear masks, socially distance whenever they around others, avoid social gatherings, and take other hygienic measures. Otherwise, Utah could replay the tragedies we saw in Italy, New York and other areas last spring when hospitals were completely inundated with COVID-19 patients.
Do Hospitals Make More Money on COVID Patients?
Some have alleged hospitals make more money treating COVID patients, which incentivizes them to take more COVID patients or to diagnose patients with two or more conditions including COVID as a primary COVID diagnosis. Hospitals and doctors will be reimbursed for treating COVID cases by health insurance companies, Medicare and Medicaid based on established rates of payment. There is no upcharge or financial gain for treating a COVID patient or classifying a patient with a primary COVID diagnosis. Hospitals are urging people to avoid contracting COVID so they don’t need hospital care. Hospitals want fewer not more COVID cases.