Workplace Resources
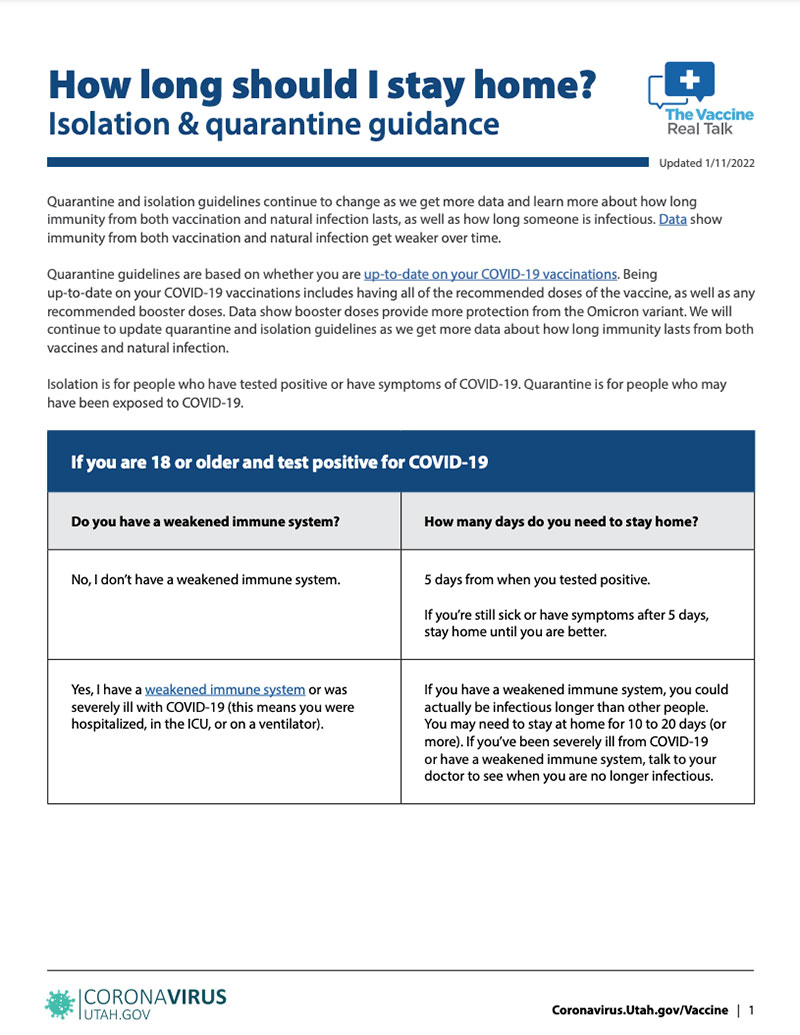
Confused about the new quarantine and isolation guidelines? Learn how long you need to stay home after testing positive or being exposed to COVID-19.
There is a new online reporting system for businesses. You can use this link to confidentially report all positive COVID-19 cases and any close worksite contacts. https://redcap.
The CDC Community Levels can help businesses and employers make decisions about when to recommend employees and patrons or clients wear masks. If your community is at a "high" level, it's recommended to wear masks indoors.
COVID-19 Business Manual
(Updated 1/20/2022)
The COVID-19 Business Manual is a step-by-step plan from the Utah Department of Health to protect your business and prevent the spread of COVID-19. It is important to look at how your business operates and make a plan to make your worksite healthier. The manual has up-to-date recommendations from the UDOH, CDC, OHSA, and U.S. Department of Labor.
Some of the information you will find in the manual:
- Keeping your business open and what you should do if an employee is exposed to or tests positive for COVID-19
- Answers to questions business owners have about requirements for quarantine and isolation, sick leave, and tax credits
- Cleaning after a positive case of COVID-19
- Testing employees for COVID-19
- How to protect your worksite, operations, and employees
- Essential and critical infrastructure sector employees
Information for child care centers
Child care facilities are an essential part of our economy and families’ lives. Decisions about how to respond to COVID-19 in child care facilities should be made in order to keep these businesses open and protect both the immediate and long-term health and safety of the children and employees.
Learn more
Employee exposure scenarios
- An employee is exposed to a coworker who tests positive for COVID-19.
- An employee lives with someone who tests positive for COVID-19.
- An employee has a family member who was exposed to COVID-19 but the employee was not exposed to the person who tested positive.
- An employee is exposed to someone who tests positive for COVID-19 in her personal life.
- An employee is exposed to someone who tests positive for COVID-19 but the employee has already had COVID-19 within the last 90 days (about 3 months).
- An employee is exposed to someone who tests positive for COVID-19 but the employee has already had COVID-19 more than 90 days ago (about 3 months).
- An essential employee is exposed to a coworker who tests positive for COVID-19. There is no one else who can do the job of the essential employee who was exposed.
- An essential employee is exposed to a coworker who tests positive for COVID-19. Other workers can do the job of the essential employee who was exposed.
- An employee who has had her COVID-19 booster dose is exposed to someone who tests positive for COVID-19.
- An employee who hasn’t had her COVID-19 booster dose yet is exposed to someone who tests positive for COVID-19.

Healthy customers. Healthy employees. Healthy economy.
The COVID-19 pandemic has taken a tremendous toll on individuals, families, communities, and businesses. Economic activity and health outcomes are tightly connected. Economies thrive when people feel and are safe.
One of the simplest ways to protect lives and livelihoods is by wearing a face mask. Nearly all reputable medical and scientific organizations agree that masks are an effective way to stop the spread of COVID-19.* A recent study by the Centers for Disease Control and Prevention showed not only do masks protect other people from getting infected with the virus that causes COVID-19, but that masks can also be protective for the person wearing a mask.** Mask-wearing decreases the number of COVID-19 cases, increases consumer mobility, and increases consumer spending.
* https://pws.byu.edu/covid-19-and-masks
** https://www.cdc.gov/coronavirus/2019-ncov/more/masking-science-sars-cov2.html
How long does an employee need to stay home after testing positive for COVID-19?
Stay home if you have symptoms of COVID-19 or test positive, even if you are vaccinated or had COVID before. Stay at home except to get medical care. You should not come to the child care facility, work, travel, or go to other activities or gatherings.
If you have symptoms, stay home until:
- You have been fever-free for 24 hours without using medicine to lower your fever,
- Your symptoms have improved for 24 hours,
- It has been at least 5 days from the day you were tested. The day you test positive is called day 0. Stay home until it has been 5 full days after you test positive (days 1-5). You must stay home for at least 5 days.
You may need to stay at home longer than 5 days if your symptoms have not gotten better. Some symptoms, like losing your sense of taste or smell, can last for weeks or months even though you are no longer infectious and don’t need to stay home anymore. Learn more here.
Wear a well-fitting mask around others and in public for another 5 more days after you end your isolation at home.
If you never had symptoms, stay home until:
- It has been at least 5 days since the day you were tested. The day you test positive is called day 0. Stay home until it has been 5 full days after you test positive (days 1-5). You must stay home for at least 5 days.
If you get sick or develop symptoms, your 5-day isolation at home starts over. Learn more here.
Wear a well-fitting mask around others and in public for another 5 more days after you end your isolation at home.
You are infectious and can spread the virus to others starting up to 2 days before you first had symptoms until your isolation period is over. If you never had symptoms, you are infectious starting 2 days before the day you were tested for COVID-19. Anyone who came into close contact with you during this time is exposed.

How long does an employee need to stay home after being exposed to COVID-19?
Everyone needs to wear a well-fitting mask around other people for 10 days after they are exposed to someone with COVID-19.
Some people may also need to quarantine at home for 5 days. You don’t need to quarantine at home if you tested positive for COVID-19 in the last 90 days (about 3 months). You also don’t need to quarantine at home if you are up-to-date with your COVID-19 vaccinations. This means you’ve had:
- A booster dose of any COVID-19 vaccine, or
- A 2nd dose of the Pfizer or Moderna COVID-19 vaccine in the last 5 months, or
- A Johnson & Johnson COVID-19 vaccine in the last 2 months.
- Children younger than 18 are considered up-to-date if they’ve had 2 doses of the Pfizer COVID-19 vaccine. A booster dose is not included in the definition of up-to-date yet for children.

You need to quarantine at home for 5 days if:
- You are unvaccinated. This means you haven’t had any doses of a COVID-19 vaccine.
- You are not up-to-date with your COVID-19 vaccinations.
- It’s been more than 90 days since you tested positive for COVID-19 and you’re not up-to-date with your vaccinations.
If you can’t wear a mask after being exposed or after ending a 5-day quarantine at home, the CDC recommends you stay at home for 10 days instead of 5.
We also recommend you get tested 5 days after your last close contact with the person who has COVID-19 to make sure you’re not possibly spreading the virus to others. If you test positive or develop symptoms, isolate at home right away. If it’s been less than 90 days (about 3 months) since you first tested positive for COVID-19 and you don’t have any new symptoms, you don’t need to get tested again during this 90-day timeframe.
Watch for symptoms of COVID-19 and get tested if you get sick. It is important to keep checking for symptoms and take extra safety precautions.

How long does an employee need to stay home if they are living with someone who tests positive COVID-19?
People who live with someone who has COVID-19 are called household contacts. Household contacts are at a much higher risk of getting infected with the virus.
You will need to quarantine at home for at least 5 days if you live with someone who has COVID-19 and you are unvaccinated, or not up-to-date with your COVID-19 vaccinations, or it’s been more than 90 days since you had COVID-19. It can be very hard to stay away from people who have COVID-19 and live in your home. This means you may need to quarantine at home longer than 5 days if you can’t stay away from the person who has COVID-19. Every time you come into close contact with the person who tested positive while they are still in isolation, your quarantine starts over.
Keep yourself and others in the house safe by wearing a mask around the person who has COVID-19. Get tested if you get sick or have symptoms.

Do employees have to quarantine at home if they’ve already had COVID-19?
If it has been less than 90 days (about 3 months) since you tested positive for COVID-19, you don’t have to quarantine at home. The CDC and Utah Department of Health recommends you not get tested if it’s been less than 90 days (about 3 months) since you first tested positive for COVID-19, as long as you don’t have new or worsening symptoms. Call a doctor to see if you may have gotten reinfected if you have new or worse symptoms during this 90-day timeframe. We know there is a small chance you could get reinfected with COVID. Some people will continue to test positive even though they are no longer able to spread the virus to others. However, if it’s been more than 90 days since you tested positive and you are not up-to-date with your COVID-19 vaccinations, you need to quarantine at home and get tested 5 days after your exposure.
You should follow these guidelines for 10 days from the date of your last exposure:
- Check for symptoms of COVID-19 every day.
- Wear a well-fitting mask when you are around people you don’t live with.
- If you get sick or have symptoms of COVID-19, isolate and call a doctor or healthcare provider to determine if you should get tested for COVID-19 again.

Take these safety precautions after being exposed to COVID-19
- Limit the number of visitors to your home while you are in quarantine.
- Wear a mask around others. It’s important to wear a mask in public and around others until it has been 10 days since you were exposed to COVID-19. Avoid going to places where it is hard to wear a mask during these 10 days, such as a gym or restaurant.
- Check for symptoms of COVID-19 every day for 10 days after your exposure, including taking your temperature if possible. A helpful booklet called, “What to do if you are in quarantine or isolation” can help you know how to check your symptoms and what to do. Get tested right away if you have symptoms of COVID-19 during quarantine.
- Get tested at least 5 days after you last had close contact with the person who has COVID-19. If you test negative, you can leave your home as long as you wear a mask around others. If you test positive, isolate at home.
- Stay away from people who are immunocompromised or at higher risk for getting very sick from COVID-19. You should not visit a long-term care facility, nursing home, or other high risk setting until it has been at least 10 days since you were exposed to COVID-19.
- Don’t travel until your quarantine is over. Get tested at least 5 days after you were exposed and make sure your test result is negative before traveling. Don’t travel if you have symptoms of COVID-19. Wear a mask around others if you travel.


Get more information about:
Healthy customers. Healthy employees. Healthy economy.
Keeping your business open if an employee is exposed to or tests positive for COVID-19
- What do we know about how COVID-19 is spread?
- What is the difference between quarantine and isolation?
- Safety precautions for people who have been exposed to someone with COVID-19
- If an employee tests positive for COVID-19, do I need to shut down my business?
- How long should employees stay home after testing positive or being exposed to COVID-19?
- How long do employees need to quarantine at home if they are living with someone who has COVID-19?
- Do employees have to quarantine if they’ve already had COVID-19?
- Should employees provide proof of a negative COVID-19 test result before returning to work?
- Essential or critical infrastructure employees
- Are my employees required to get vaccinated?
- Do employees still need to isolate if they test positive for COVID-19 after being vaccinated?
Case investigations and contact tracing
- Will the health department call my business or agency if an employee tests positive?
- Is there a law that requires me to give the health department information about employees who may have been exposed to or tested positive for COVID-19?
- You may be asked to do your own contact tracing
- How do I protect employee confidentiality during contact tracing?
- What does close contact mean?
- Understanding the date of exposure
- How to determine when someone can end quarantine
- What is the difference between cleaning, sanitizing, and disinfecting?
- Cleaning tips for employees
- Cleaning products
- How to clean different surfaces
- Personal protective equipment (PPE) for cleaning staff
- Cleaning after a positive case of COVID-19
- Engineering and ventilation controls
- Recommendations for specific areas and spaces at your workplace
- Sick leave
- Staffing and work schedules
- Keep operations going
- Meetings and gatherings
- Hygiene
- Face masks
- Physical spaces
- Sick employees
- Engineering and ventilation controls
- Protect your building water system and devices after a long shutdown